Speciality - Knee
About Knee joint
The knee joint is a type of a hinge joint and has three parts where the thigh bone (femur) meets the large shin bone (tibia) to form the main knee joint. The kneecap (patella) joins the front of the femur to form the patellofemoral joint. The patella glides in front of the femur during movements and protects the front of the knee joint.
The knee joint is surrounded by a capsule with ligaments on each side of the joint (collateral ligaments) as well as within the joint (cruciate ligaments). The function of these ligaments is to provide stability to the knee joint during its complex movements. The collateral ligaments run along the sides of the knee and limit the sideways motion of the knee. The anterior cruciate ligament (ACL) functions to limit rotation and forward motion of the tibia whereas the posterior cruciate ligament (PCL) located just behind the ACL limits the backward motion of the tibia.
The meniscus is a thick cartilage cushion between the joint formed by the femur and tibia. The meniscus makes the joint surfaces more congruent, acts as a shock absorber and also plays a little part in the stability of the knee joint. The large muscle in the front of the thigh, quadriceps muscle, extend (straighten) the knee joint. In the back of the thigh, the hamstring muscles flex (bend) the knee.
The knee is a weight bearing joint and allows complex movements mainly flexion, extension and a small degree of rotation. The structures both inside and outside the knee work in harmony to provide easy and stable movements at this joint during our daily activities including sports. This is one of commonest joints to be injured due to accidents or sports injuries and is a common reason for many orthopaedic consultations. Knee pain can also be the source of referred pain (problem somewhere else) from hip, spine or ankle. Your doctor will take a detailed history from you and then examine you thoroughly to establish the exact reason for your knee pain.
Investigations that are commonly performed for knee pain are X rays, CT scans, MRI scans, Ultrasounds and sometimes blood tests.
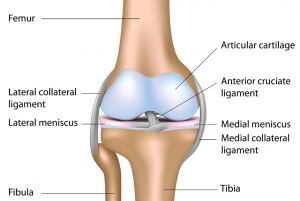 Figure: Different parts of the knee joint
Figure: Different parts of the knee joint
Osteoarthritis of knee joint
This is the commonest cause of knee pain in patient above the age of 50 years and is a degenerative condition. This occurs when the shiny smooth cartilage (Hyaline cartilage) covering the ends of the femur (thigh bone), tibia (shin bone) and patella (knee cap) wears away and the bone ends directly rub against each other causing pain, limitation of movements and disability. All of these symptoms will eventually effect the quality of life of the patient stopping them from their routine activities.
Initial management involves simple pain killers, anti-inflammatory medications, life style modifications and physiotherapy, weight loss and occasionally joint injections. When all these non- operative measures fail to control the patient’s symptoms, the doctor will advise you to consider knee replacement surgery. This is a commonly performed procedure with very good success rates and benefits patients who have severe knee pain limiting their daily activities including walking, climbing stairs, getting in and out of bed and chair.
It is important to understand that this condition mainly effects patients above the age of 50 years and hence age is not a contra indication to surgery. Following medical assessment your doctor may advise you to consider knee replacement surgery if you wish to resume normal activities and mobilise pain free.
Link for further reading: https://www.nhs.uk/conditions/osteoarthritis/Pages/Introduction.aspx
 Figure 1: Diagrammatic representation of a normal knee and a knee joint with osteoarthritis
Figure 1: Diagrammatic representation of a normal knee and a knee joint with osteoarthritis
 Figure 2: Plain radiographs showing a normal knee on the left and advanced osteoarthritis in another knee joint on the right side of the picture
Figure 2: Plain radiographs showing a normal knee on the left and advanced osteoarthritis in another knee joint on the right side of the picture
Meniscus tears
Knee joint meniscus
The knee joint has two menisci (medial and lateral) which are crescent shaped and make the joint congruent to allow for a rounded femur end to glide on a relatively flat tibial surface. This cartilage along with acting as a shock absorber of the knee also play a role in providing stability to the knee joint. Meniscal pain worsens on twisting/turning on the affected joint and is often painful when squatting or on deep knee bends
Meniscus injury
The knee is one of the most commonly injured joints particularly in sports and road traffic accidents and meniscus is perhaps the commonest cartilage injury of the knee. The typical injury pattern is a forceful knee movement whilst weight bearing on the same leg and it may tear fully or partially. They can also occur due to repeated small injuries to the cartilage or to wear and tear (degeneration) of the meniscal cartilage in older people. In severe injuries, there may be a combination of ligament injuries (Cruciate or collateral ligaments).
Meniscal cartilage does not heal well once on its own because of its precarious blood supply and hence most of them will need surgery.
Symptoms of a meniscus tear
Patients with a meniscus tear can have a variety of symptoms including pain, locking of the knee, swelling, pain on full straightening the knee or bending it beyond 90 degrees or most commonly on squatting or sitting in prayers. These symptoms can be varied in intensity and maybe intermittent. Some patients will have meniscal tears without any pain, especially in patients who have degenerate tears due to repeated small injuries over the years and the only symptom can be a swelling or effusion in the knee joint.
Treatment of a meniscus tear
Treatment of a meniscus tear will depend on the nature of injury. In the early phase (acute) after injury, you may need some rest, ice packing, pain killers including anti-inflammatory medications and compression.
After consultation with your surgeon and clinical assessment, you will most probably need a MRI scan to assess the nature and extent of injury which will guide further management. You may be referred for physiotherapy to help with the swelling, regaining range of movement of the knee and strengthening your muscles around the knee.
However, if your knee is locked or you are having deep pain, persistent painful swelling or mechanical symptoms your doctor may advise arthroscopic surgery (keyhole). During surgery, it may be possible to repair the tear but in some cases this is not possible and the tear in this case is trimmed or cut out to even up the surface.
Following surgery, you will be referred for physiotherapy to keep the knee joint active and strengthen the surrounding muscles.
Asymptomatic meniscus tears can be left alone and do not need any surgical intervention.
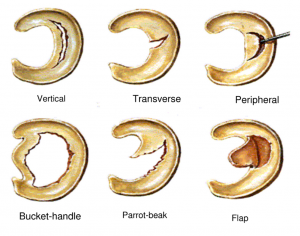 Figure: Different types of meniscus tears based on configuration of tear
Figure: Different types of meniscus tears based on configuration of tear
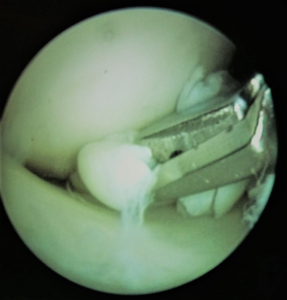 Figure: Arthroscopic (Keyhole) surgery of a tear of medial meniscus which was causing locking of the knee joint.
Figure: Arthroscopic (Keyhole) surgery of a tear of medial meniscus which was causing locking of the knee joint.
Cruciate ligament injury
Anterior cruciate ligament tear
Anterior cruciate ligament (ACL) is one of the two strong ligaments inside the knee joint. It provides stability to the knee joint during daily routine and sporting activities where it prevents the tibia (shin bone) from gliding in front of the knee joint and also prevents the twisting movement of the knee.
This ligament can be ruptured during sports activities and it rarely heals itself and the knee may give way. Regular giving way can lead to secondary damage to the knee and lead to early development of arthritis.
Not everyone will need reconstruction of this ligament and your doctor after clinical assessment will decide with you about the best course of action. There is some emerging evidence that long term focussed ACL rehabilitation can lead to return to normal activities without surgery. If however, your knee gives way on you regularly, you will need to consider reconstruction of the ACL to return to normal activities and prevent further damage.
A ligament graft is required using material taken from the front of the knee or from the hamstring tendons behind the knee, both of which are able to re-grow to a large extent. Successful ACL reconstruction will mean your knee will no longer give way and you can return to sport and everyday activities.
 Figure: Arthroscopic view of the left knee joint, demonstrating a torn anterior cruciate ligament (Empty wall sign).
Figure: Arthroscopic view of the left knee joint, demonstrating a torn anterior cruciate ligament (Empty wall sign).
Tendinitis
The knee joint is surrounded by various muscles, tendons and ligaments. Any of these structures can get inflamed and become painful or get injured in any sporting activities.
Some of these conditions that effect the knee are patellar tendinopathies, supra patellar bursitis, pre patellar bursitis, infra patellar bursitis, pes anserine bursitis, Osgood Schlatters disease and Hoofas syndrome. Any of these conditions can cause pain and swelling in and around the knee. It is important that your doctor examines you in detail after a good history, as many of these conditions are readily treatable. You may need X rays, Ultrasound or an MRI scan during your work up. Following consultation and investigations, your doctor will advise you about the best course of action. Most of these conditions are treatable with simple pain killers, anti-inflammatory medications, ice packing, physiotherapy and occasionally targeted injections in the painful spots. Surgery is very rarely required in the treatment of these conditions.
Management of knee pain
This will depend on the cause of knee pain. The approach to management of knee pain is usually multi modal and may involve simple oral medications, physiotherapy, cryotherapy and occasionally injections. Certain conditions like advanced arthritis not responding to pain killers, symptomatic meniscus and cruciate ligament tears will need surgery. Your doctor will explain each of these procedures to you and discuss any alternative options if available.
Knee joint injection
This is one of the commonest areas to be injected. The indications for injection into the knee joint is usually inflammation which could be due to osteoarthritis, rheumatoid arthritis or traumatic etc. They can provide good pain relief in patients who have moderate osteoarthritis not responding well to oral analgesia or in patients who have advanced arthritis and are not fit or willing for surgery. Sometimes specific areas around tendons need to be injected for inflammation such as around the patella tendon. These injections are usually performed in the clinic after consultation and discussion with your doctor.
The pain can sometimes increase for the first day or so after the injection and this is not unusual. However, if you have any concerns at all after the injection, you should come back and see your doctor.
Knee Treatment
- Kneecap (patella) stabilisation surgery
- Surgical procedures
- Anterior Cruciate ligament reconstruction
- Knee arthroscopy surgery
- Knee cap joint replacement surgery
- Knee realignment (osteotomy) surgery
- Knee replacement (partial) surgery
- Knee replacement surgery
- Kneecap Joint Replacement Surgery
- Knee cartilage surgery
- Meniscus repair surgery
- Meniscal Scaffold
- Meniscal Allograft
