Speciality - Hip
About Hip Joint
The hip joint is one of the largest joints in the human body and is a ball and socket type joint. The surfaces of the ball and socket part are covered by a specialized type of cartilage which is one of the smoothest surfaces known to man. The purpose of this cartilage is to reduce friction between this joint to allow free movements. When this cartilage is worn out, the surfaces become rough and this in turn causes pain, stiffness and reduction in activities.
Conditions that effect hip joint?
The commonest condition effecting the hip joint causing all these symptoms is osteoarthritis. A variety of other conditions can affect the hip causing similar symptoms including rheumatoid arthritis, hip fractures and dislocations, pelvic fractures, avascular necrosis, ankylosing spondylitis and occasionally infections and tumours.
Osteoarthritis of the hip joint?
This happens when the smooth cartilage at the ends of the bones forming the hip joint wears off causing pain and stiffness. When this cartilage is completely worn off, bone ends rub against each other causing significant pain, discomfort and loss of mobility effecting the quality of life of the patients. This happens commonly in patients over the age of 50 years but can happen sooner depending on the cause.
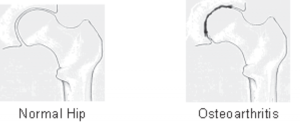 Figure: Osteoarthritis of the hip joint
Figure: Osteoarthritis of the hip joint
Hip fracture
This is one of commonest injuries dealt by orthopaedic surgeons and happens usually in patients beyond the age of 60 years as their bones are weak and fragile (Osteoporosis or osteopenia). Patients usually have a fall from a standing height and present with pain in and around the hip joint and a shortened and rotated leg on the involved side. As expected elderly patients may have numerous other medical problems which makes this injury by no means just a surgical concern. Its effective management requires the co-ordinated application of medical, surgical, anaesthetic and multidisciplinary rehabilitation skills and a comprehensive approach covering the full time course of the condition from presentation to subsequent follow-up, including the transition from hospital back to home.
Other patients who can have hip fracture are people with weak bones due to other medical problems such as a tumour (called pathological fracture) and younger patients who are involved in major trauma, such as road traffic accidents. On presentation, if there is a concern of hip fracture, after initial management, patients are sent for x rays which will confirm or refute the presence of a hip fracture (Figure 1). Based on the findings, further management is planned. These fractures are exclusively managed with surgery unless the patient is extremely unwell and cannot tolerate an anaesthetic for surgery or patients refuse surgery. There is undebatable and clear scientific evidence that prompt surgical intervention reduces the morbidity and mortality associated with this injury as otherwise patients will be bed bound and will develop numerous complications including chest infection, bed sores, urinary tract infection, clots in legs which can propagate into the lungs, heart or brain leading to pulmonary embolism, heart attack or stroke which are eventually fatal. Prompt surgery will reduce pain and help early mobilisation of these patients reducing the risk of these aforementioned complications.
 Figure: X-ray of Right hip confirms the presence of a displaced fracture.
Figure: X-ray of Right hip confirms the presence of a displaced fracture.
Depending on the type and location of fracture, surgical management is planned (Figure 2). These fractures are usually fixed with different implants if they are extracapsular, commonly a Dynamic hip screw (DHS) or an Intra medullary nail as the blood supply is not disrupted. Whereas with intra capsular fractures, as the blood supply is disrupted the fractured part is usually replaced by a prosthesis where either a half hip replacement or total hip replacement is performed. Only in completely undisplaced intracapsular hip fractures or younger patients, these fractures are fixed in an attempt to get them to heal. This is however, not always successful but is recommended to be attempted in this select group of patients.
Recent scientific evidence and guidelines suggest that elderly patients with intracapsular hip fracture who can withstand an anaesthetic and are mobile, do very well with a total hip replacement in comparison with hemiarthroplasty (half hip replacement).
Link: https://www.nice.org.uk/guidance/cg124.
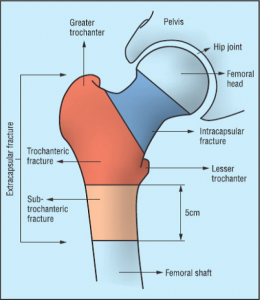 Figure: Schematic picture showing the different types of fractures.
Figure: Schematic picture showing the different types of fractures.
Hip pain management
Management of hip pain will depend on the cause and the approach is usually multimodal. This involves the use of various different pain killers taken orally and occasionally delivered via injections into the flesh (intra muscular) or blood vessels (Intravenous). In the acute situations, sometimes nerve blocks can be used to reduce the pain. For chronic conditions, life style modifications and physiotherapy can also be beneficial. In certain conditions injections into the hip joints can be used to help reduce the pain. For surgical causes of pain, surgery will alleviate the pain once performed.
Injection
This is one of the common joints to be injected. The indication for injection is usually inflammation which can be due to osteoarthritis, rheumatoid arthritis, impingement or trauma. They can provide good pain relief in patients who have moderate osteoarthritis not responding well to oral analgesia or in patients who have advanced arthritis and are not fit or willing for surgery.
These injections are performed with the help of an x ray machine and is a day case procedure and does not need general anaesthesia. The pain can sometimes increase for the first day or so after the injection and this is not unusual. However, if you have any concerns at all after the injection, you should come back and see your doctor. This injection can be repeated if needed after consultation with your doctor.
